Talk Overview
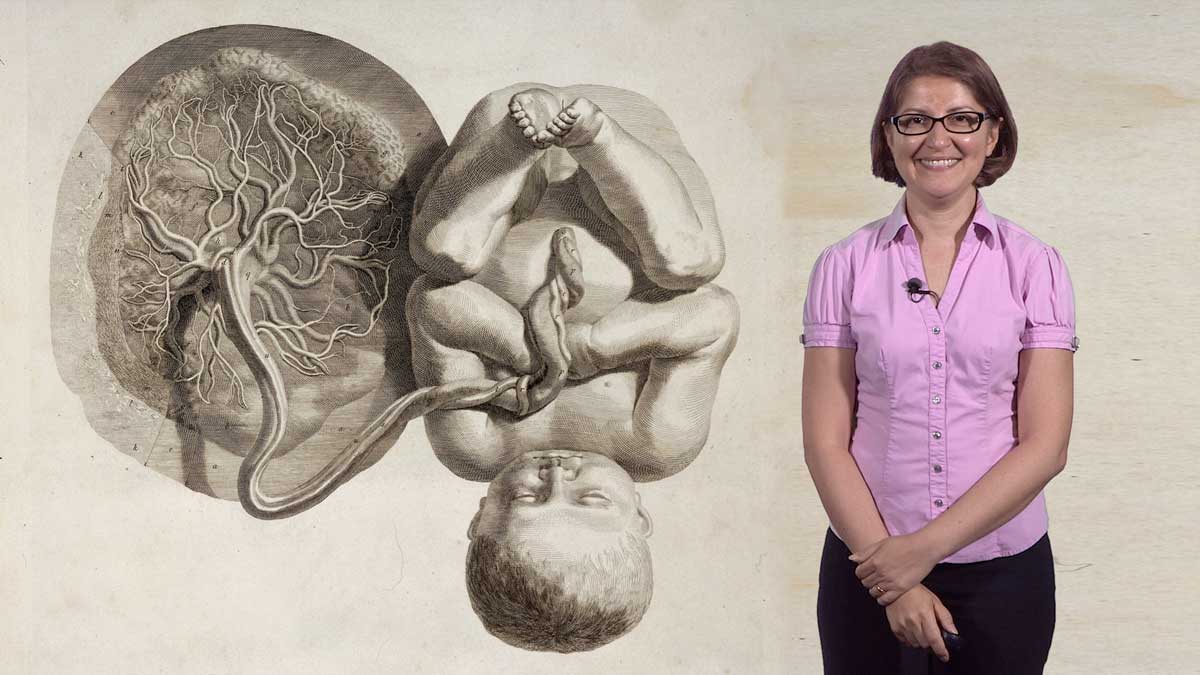
Dr. Fuchs begins her talk with a brief history of stem cells including the discovery in the 1970s that adult skin stem cells could be cultured in vitro indefinitely. This early work provided the foundation for later advances in embryonic stem cell (ESC) culture. ESCs are special because they can generate all the different tissues of the body, thus providing great potential for use in regenerative medicine. The use of ESCs is controversial, however, so scientists have developed ways of generating pluripotent stem cells that do not use embryonic tissue. Fuchs reviews methods such as nuclear transfer and the generation of induced pluripotent stem cells (iPSCs) by reprogramming adult somatic cells. Cells generated by these methods may be used for drug and therapy screening and they may provide treatments for human diseases such as macular degeneration, Parkinson’s and other degenerative diseases.
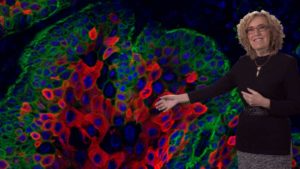
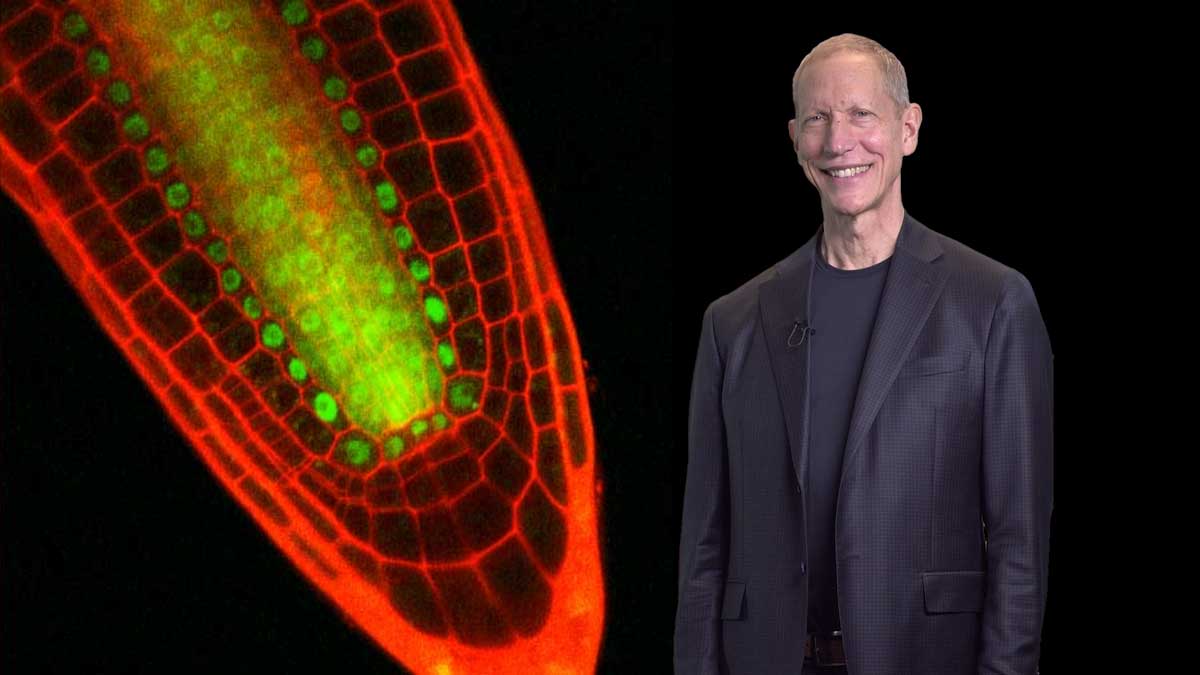
In her second talk, Fuchs focuses primarily on studies of adult skin stem cells. Adult stem cells have the ability to make more stem cells and to generate the cells of a differentiated tissue. Skin stem cells can replenish the epidermis and make hair follicle cells. Skin grown in culture from just a few skin stem cells can be used to treat burn patients or replace damaged corneal epithelium. Stem cells reside in specific niches or microenvironments and signals from the niche determine whether a stem cell is going to be quiescent or make tissue. Fuchs’ lab has studied hair follicle stem cells for many years and has identified the signals that activate hair follicle stem cells as well as the specific set of transcription factors that are upregulated in the activated stem cells. They have shown that many of the genes turned on during stem cell activation are regulated by super enhancers which sense the niche environment.
Squamous cell carcinomas (SCCs) are commonly occurring, dangerous cancers that may originate from skin stem cells. By developing methods to identify the stem cells that will lead to cancer, Fuchs’ lab has been able to study how these cells differ from normal skin stem cells. They found that the gene expression profile in normal versus cancer stem cells is very different and is likely the result of differences in the cancer stem cell niche. The tumor microenvironment may include immune cells and greater proximity to TGF-beta secreting blood vessels. Fuchs’ lab showed that cancer stem cells exposed to TGF-beta had increased expression of proteins in the glutathione metabolism pathway; the same pathway which is involved in the breakdown of chemotherapy drugs. Further studies in SCC patients, showed a strong correlation between increased mRNA levels for glutathione pathway proteins and decreased survival. These results suggest that drugs which block TGF-beta activity, in combination with other chemotherapeutics, may be an effective therapy for some SCC.
Speaker Bio
Elaine Fuchs

Elaine Fuchs is the Rebecca C. Lancefield Professor of Mammalian Cell Biology and Development at The Rockefeller University and an Investigator of the Howard Hughes Medical Institute. Her lab studies the role of skin stem cells in homeostasis and wound repair and how these processes go awry in cancer and inflammatory diseases. Fuchs received… Continue Reading









Jane says
I’m sorry but when you’re explaining the Wnt signaling, BPM, and Shh it was very confusing. Barely understood it.